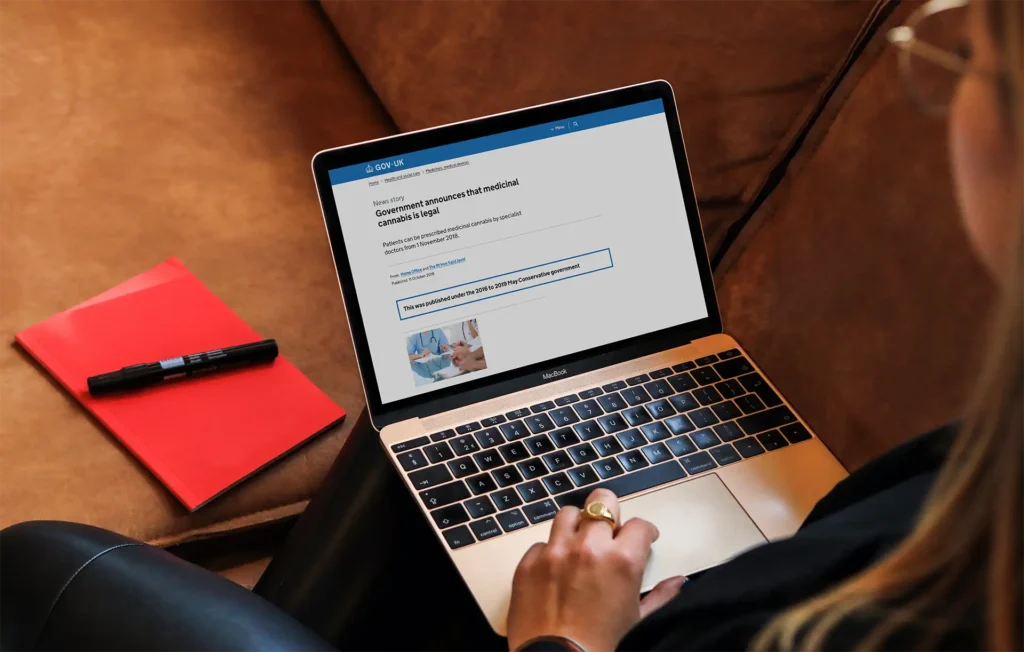
Seven years ago, on 1 November 2018, the UK took a landmark step forward by legalising medical cannabis for patients with chronic physical and mental health conditions. This November, we mark the anniversary of that decision — reflecting on how far we’ve come and where we still need to go.
Today, tens of thousands of patients in the UK have access to legal, regulated medical cannabis. For both patients and clinicians, having another option to explore in symptom management is a powerful and positive step forward.
Yet access remains uneven: limited clinical evidence, low awareness, cost, and stigma continue to pose significant challenges.
Medical Cannabis Access in the UK: The Story so Far
This timeline highlights some of the key moments since legalisation — a story of steady progress, growing understanding, and ongoing effort to make medical cannabis more accessible to all who could benefit.
November 2018
The Misuse of Drugs Regulations 2001 are amended to allow cannabis-based medical products (CBMPs) to be prescribed by specialist doctors. This change made medical cannabis legally available on prescription in the UK for the first time.
November 2019
The National Institute for Health and Care Excellence (NICE) publishes its first guidance on medical cannabis products. Although medicines such as Sativex (for spasticity in adults with multiple sclerosis) and nabilone (for chemotherapy-induced nausea and vomiting) were already licensed and available on the NHS, this guidance marks the first time NICE formally reviewed and supported their use — alongside Epidiolex for treatment-resistant epilepsy, including Lennox–Gastaut and Dravet syndromes, as well as tuberous sclerosis complex.
December 2019
Curaleaf Clinic, then known as Sapphire Medical Clinics, becomes the first private medical cannabis clinic to be registered with the Care Quality Commission (CQC) in the UK.
March 2020
Curaleaf Clinic publicly launches the UK Medical Cannabis Registry (UKMCR), the first registry of its kind in the UK, created to track how patients use medical cannabis and changes in their health and wellbeing. The UKMCR is proudly the largest registry of its kind.
March 2021
Curaleaf Clinic becomes the first medical cannabis clinic registered with Healthcare Improvement Scotland (HIS) to provide in-person consultations for patients in Scotland, expanding access beyond England for the first time. Although we are no longer registered with HIS, patients in Scotland can still access appointments virtually through our CQC-regulated service. Read more about Curaleaf Clinic’s work in Scotland here.
2021
The Home Office grants commercial cultivation licences for medical cannabis in the UK, laying early groundwork for a domestic supply chain and reducing reliance on imported products.
May 2021
The UK Medical Cannabis Registry (UKMCR) publishes its first peer-reviewed study, ‘An initial analysis of the UK Medical Cannabis Registry: Outcomes analysis of first 129 patients’. The UKMCR has gone on to publish nearly 40 additional studies, expanding the understanding of medical cannabis globally.
December 2022
The NHS introduces mandatory reporting for patients prescribed medical cannabis, creating a national record to track usage and patient outcomes, strengthening evidence-based oversight across the health system.
September 2024
Curaleaf Clinic publishes “The Hidden Dangers of Illicit Cannabis” in partnership with Manchester Metropolitan University, revealing high levels of contamination — including mould, bacteria, and heavy metals — in illegal cannabis samples. The study showcases the importance of regulated access and product safety.
October 2024
University College London and Great Ormond Street Hospital (GOSH) announce two NHS-backed clinical trials into cannabis-based medicines for treatment-resistant epilepsy in children and adults. Recruitment of around 500 patients is expected to begin in 2025 — marking the first NHS-led research of its kind in the UK.
May 2025
The London Drugs Commission publishes a major report recommending that personal possession of cannabis be decriminalised in the UK. While the proposal focuses on recreational use, the report sparks renewed national debate about cannabis policy and regulation. Read more about what this means for patients here.
June 2025
The Home Office commissions the Advisory Council on the Misuse of Drugs (ACMD) to review the impact of the 2018 legislative change. The aim is to determine whether the law change is working as intended, to identify any unexpected problems and to recommend how things could be improved going forward.
September 2025
Curaleaf Clinic and the Centre for Economics and Business Research (Cebr) publish new analysis showing private prescriptions have added £283 million to the UK economy since 2018, and that wider NHS access could unlock £13.3 billion more over the next decade. Read the full report on wider NHS access here.
November 2025
The UK marks seven years since medical cannabis was legalised for prescription.
Understanding the Barriers to Access
Despite the progress made since 2018, the ongoing challenges are well recognised:
- NHS Access: Very few prescriptions are issued through the NHS. Most patients rely on private care, creating financial strain for families – particularly those with children living with severe epilepsy.
- Clinical Confidence: Many healthcare professionals remain uncertain about prescribing due to limited formal training and slow updates to clinical guidance.
- Stigma and Awareness: Half of the UK population still doesn’t know medical cannabis is legal, and misconceptions persist among both patients and practitioners.
- Research Gaps: Although evidence is growing rapidly, further large-scale clinical studies are needed to inform NHS commissioning and reassure prescribers.
These challenges can only be addressed through collaboration — between policymakers, regulators, researchers, and clinicians — to build the evidence base, improve education, and ensure fair access for all eligible patients.
How is Curaleaf Clinic Contributing to Wider Medical Cannabis Access?
- At Curaleaf Clinic, we’re committed to expanding access to medical cannabis through:
- Research: We are passionate about research and our UK Medical Cannabis Registry now has over 40,000 patients contributing valuable data on how medical cannabis impacts their health and quality of life. This data fuels our research, with nearly 40 peer-reviewed papers published to date.
- These papers are used to educate healthcare professionals and drive legislative change, they also shape our own prescribing. Find all our published work from the UK Medical Cannabis Registry here.
- Education: We strive to educate the public and healthcare providers about medical cannabis. Our doctors and pharmacists have been at events up and down the country, and even internationally, to help inform healthcare professionals, charities, and police on medical cannabis.
- Awareness: Patient stories are powerful tools in breaking down stigma. We’re proud to have amplified patient voices across major media outlets like ITV, The Guardian, The Times, and the BBC.
Making Care More Affordable
At Curaleaf Clinic, we’ve expanded our range of appointment payment options to suit more patients.
- Pay per appointment: £50 appointments for all patients. First follow-up is free when you join the Curaleaf Access Scheme and contribute to the UK Medical Cannabis Registry.
- Monthly Subscription: spread the cost of appointments over time for just £10 per month. This covers all routine check-ups per year.
- Annual plan: save by paying upfront – £100 covers all routine appointments for the year.
- Veterans’ Access Scheme: UK veterans receive up to five free appointments per year.
The Road Ahead for Medical Cannabis in the UK
To unlock the full potential of medical cannabis in the UK, we need to see action.
Our latest research with the Centre for Economics and Business Research (Cebr) makes a compelling case for change — showing how expanded NHS access could unlock billions of pounds in economic value over the next decade.
To realise this potential, Curaleaf Clinic will continue advocating for:
- Fair NHS access for eligible patients, so medical cannabis is not limited to those who can afford private care.
- Greater education and training for healthcare professionals to increase clinical confidence and reduce stigma.
- More research investment to build on real-world evidence and inform policy reform.
Seven years on from legalisation, the UK stands at a turning point. The evidence is clear, the demand is real, and the opportunity to deliver compassionate, cost-effective care has never been greater.
Next November, we hope to have further positive change and progress to celebrate.